Introduction
Learning is a process aimed at improving knowledge, skills and attitude of the student which involves the cognitive, psychomotor and affective domains. A rapid pace of change in health care and medicine is bringing about corresponding changes in the content and process of medical education. Guidelines on medical education across the world are emphasizing on integration of medical curriculum. Integration is a learning experience that allows the learner to perceive relationships from the blocks of knowledge and develop a unified view of its basis and application. The competency-based curriculum in India, is an outcome driven curriculum, which aims that teaching does not remain in the separate academic departments and therefore calls for both horizontal and vertical integration.
Vertical integration is an intervention bridging the gap between the basic sciences and the clinical sciences. It can be achieved by exposing the students to clinical cases at an early stage. Best practices and ideas gleaned from experts and institutions across the world have documented about the conduct of early clinical exposure (ECE), which states that the students can be exposed to clinical experiences in various forms and in a variety of settings. Each institution, depending upon the means available, can adopt any of these approaches with a view to provide clinical correlation to basic sciences learning.
Exposure to the actual clinical set up and patients at an early stage helps the students to develop the right attitude and professionalism. It enhances learning in the early years of undergraduate education by playing a crucial role in development of clinical reasoning, communication skills, leadership and lifelong learning skills in a student.1
The competency based medical education curriculum in Human Anatomy has defined certain competencies in which applied anatomy of the hip joint and knee joint has been vertically integrated with the Orthopaedics.2 This study was conducted to analyse the impact and feasibility of such vertical integration through actual patient contact, by introducing first year MBBS students to clinical cases in the Orthopaedics OPD.
Materials and Methods
Study participants
First Professional MBBS students (Batch 2017-18). Only the students who volunteered to participate after sensitization about the project were included in the study.
Sampling procedure and sample size
139 students (consisting of 52.51 % females and 47.48% males). These 139 students were divided by a draw of lots into two batches, A and B, comprising 70 and 69 students respectively. Each batch was further grouped into four subgroups of 17 to 18 students (total 8 sub-groups).
Eight faculty members from both departments (Anatomy and Orthopaedics) participated in the study.
Permission and consent
Ethical approval was obtained from the Institutional Ethics Committee. Informed verbal consent was obtained from the students, after sensitizing them to the ECE module and explaining the methodology in detail. During this time the students were also sensitized about perception, reflections and the importance of their honest and critical feedback.
Preparation of tools
Modules on ECE of hip and knee joint were prepared by the core team which consisted of the experts from the subject and medical education. This core team also designed a facilitator’s guide which was a framework to be provided to clinicians for the conduct of ECE sessions. It specified the exact steps to be followed with the aim of guiding the facilitator to limit his content of their discussion and examination of the cases to the applied of anatomy of the topic thereby ensuring that the discussion remained confined to the level of a first year undergraduate student.
The faculty from both the departments were then sensitized to the ECE module by focussed group discussion (FGD) and the facilitator's guide.
A student feedback questionnaire was designed and validated by taking the opinion of experts and testing it on 10 medical students of batch 2016 (not included in the study). Student observation guides and class tests with 20 MCQ’s each for hip and knee joint were designed, keeping in mind the desired knowledge outcomes and the content to be covered during the sessions. A faculty feedback questionnaire was also prepared and validated by subject/medical education experts.
Conduct of the training programme
A didactic lecture on the anatomy of the hip joint was conducted for the entire class, leaving out only the applied aspect of the topic. For the implementation of the module, Batch B was taught the applied anatomy of hip joint in the practical class in anatomy department, the same day. On the other hand, the students of Batch A were given a brief introduction to the observation guide and were taken to the Orthopaedics OPD.
In the OPD, the students of Batch A were divided into the 4 subgroups (as explained earlier) and each sub-group was turn-wise shown a case of osteoarthritis of hip joint, a case of fracture neck femur, a case of post-surgical total hip replacement and a case of avascular necrosis of head of femur. Each case had an assigned facilitator (from Orthopaedics department) who examined the patients step by step, while the students observed the examination. The facilitators also discussed the findings of each case and the investigation reports with the students. On the next day a multiple choice question based class test on hip joint (about which students had been informed earlier) was conducted for all the participants (Batch A and Batch B).
The following week, the similar procedure was repeated for knee joint; but now students of batch B were taken to Orthopaedics OPD while the students of batch A learnt the applied anatomy of the knee joint in the Anatomy department. The students of Batch B were shown a case of osteoarthritis of knee joint, a case of tear of medial meniscus, a case of postsurgical total knee replacement and a case of patellar fracture. This was similarly followed by an MCQ based class test on the next day. After the class test, student perceptions and feedback regarding the ECE sessions were also obtained.
Evaluation of the training program
Perceptions by students on their experience with this module of ECE was obtained on a 5-point Likert scale with 10 items ranging from strongly agree = 5 to strongly disagree =1. The students were also asked to reflect on this module by answering the two open ended questions
Describe any two good points about the session on ECE.
Give suggestions for improvement of the session on ECE.
MCQ based class test of the students was taken to compare the difference of knowledge acquired by the exposure to early clinics compared with the knowledge of nonexposed group taught by traditional teaching method.
Perceptions by the participating faculty on their experience with this module of conducting ECE was also taken on a similar pattern as that for students.
Informal feedback was also obtained on completion of the module from the faculty facilitators of Anatomy and Orthopaedics, mainly for logistic and administrative purposes.
Data analysis
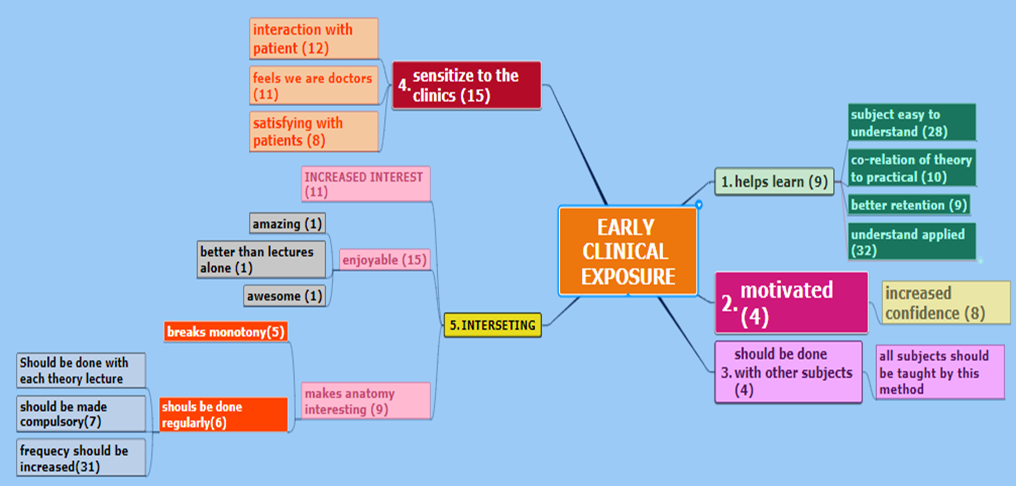
The student feedback was analysed quantitatively on Microsoft office Excel (2010) and Graph Pad software. Percentages of the responses to items on likert scale were calculated and the descriptive statistics included median to compare the proportions. For qualitative analysis the responses were tabulated with the frequency of each type of response to the open-ended questions. Then the themes were identified and a thematic tree was prepared. The responses were also categorized according to the domains of learning that it affected. In case of faculty feedback, the size of the sample for this project was only eight faculty members so the responses were kept only as numbers and not converted to percentages.
The satisfaction index was calculated from the Liker scale on the feedback questionnaire for each item, separately for both for the students and faculty. The Satisfaction Index3 is the opinion about factors related to the academic and non-academic form of a satisfaction. Student satisfaction here indicates how much the students are satisfied with the session on ECE.
For the MCQ based test, the mean, standard deviation (SD), 95% confidence interval (CI) of marks obtained by exposed and the exposed group were calculated. Unpaired t test results for the scores of exposed and nonexposed groups for the hip joint and knee joint were calculated separately and then for combined (hip joint and knee joint) to evaluate for any statistical significance.
Results
The students perceived the early clinical exposure module very well. 71.9% of the students agreed that other topics in anatomy should be taught by this method of ECE and 74.1% students wanted that ECE should be used as a method of teaching learning along with traditional teaching methods in Anatomy.
Table 1
Perception of student feedback (numbers-’n’ and percentages) with median and satisfaction index
Table 2
Perception of faculty feedback (numbers-’n’ and percentages) with Median and satisfaction index
Table 3
Classification of responses of students to open ended questions
Table 4
Hip joint MCQ test marks: Comparison of exposed and non-exposed
|
|
Exposed |
Non exposed |
Difference between the mean with 95% CI |
t value (df) |
p value |
|
Mean |
9.96 |
9.78 |
0.18 (-0.94to 1.31.) |
t=0.3284 df = 118 |
0.7432 |
|
SD |
3.16 |
3.02 |
|||
|
N |
53 |
67 |
Table 5
Knee joint MCQ test marks: Comparison of exposed and non-exposed
|
|
Exposed |
Non exposed |
Difference between the mean with 95% CI |
t value (df) |
p value |
|
Mean |
7.81 |
7.28 |
0.53 (-1.56 to 0.50.) |
t = 1.0249 df = 108 |
0.3077 |
|
SD |
2.84 |
2.50 |
|||
|
N |
42 |
68 |
Table 6
Mean marks of exposed and non-exposed groups
|
Test topic |
Exposed |
Non exposed |
|
Hip Joint |
9.96 |
9.78 |
|
Knee Joint |
7.81 |
7.28 |
|
Combined (both tests together) |
9.01 |
8.52 |
Table 7
Combined both MCQ tests marks: Comparison of exposed and non-exposed
|
|
Exposed |
Non exposed |
Difference between the mean with 95% CI |
t value (df) |
p value |
|
Mean |
9.01 |
8.52 |
0.49 (-0.33 to 1.31) |
t = 1.1853 df = 228 |
0.2371 |
|
SD |
3.19 |
3.03 |
|||
|
N |
95 |
135 |
The score of the students when exposed to ECE using Clinical OPD has performed slightly better with mean of 9.01 marks out of 20, as compared to when they were not exposed to Clinical OPD, but were taught by traditional method of teaching, where the mean is 8.52 marks out of 20. This difference between the two values is not statistically significant with p > 0.05.
Discussion
The module of ECE was acceptable to the students and had an impact to the extent that 58.3% of the students agreed that ECE had helped them in understanding of applied anatomy of the topic. This is similar to the findings by Ramachandran K who concluded that students understood clinical anatomy better with ECE.4 61.9% of the students agreed that the method of conducting ECE was an enjoyable method for learning which is comparable to the findings in a previous study in which 69% students found ECE as an exciting method. 71.5% of students in the present study were in favour of ECE being conducted for other topics which is similar to the findings of Chiari et al.5 Only 47.5% of students after the intervention in our case agreed that ECE helped them in better assimilation of knowledge on the topic whereas in a previous study more than 90% of the students agreed that attending ECE sessions helped in better retention of topic.6 Similar to conclusion by Das P et al., the students in our study also expected the department to follow this method of ECE for other topics of Anatomy.7 68.3 % students said that ECE should be used as a method of teaching learning along with regular lectures in other subjects whereas 89.7% student showed eagerness to attend more of such ECE programs. Improved learning as a result of exposure to the clinical OPD in the preclinical year and that it has helped the students to be confident about their profession, is a finding similar to a previous study which reported that ECE increases students’ interest in becoming a doctor.8
The median value on the Likert scale for the item that ECE helped the students to be sensitized to the clinical setting is 5, which is similar to the report by Chari S. et al. who also obtained a median value of 5 in their finding on sensitization of students to clinics by ECE.3 Analysis of the open ended questions showed that the students’ interest and motivation for the learning of the subject increased after ECE which was similar to previous findings by many other authors.4, 8, 9 As with previous studies,4, 7 the faculty facilitators in our study also felt that implementation of an ECE module is time consuming and needs more manpower.
In the present study, the difference in scores of the exposed and nonexposed groups was not significant though the mean score of exposed group was higher than the nonexposed group. This is in contrast to the findings of a previous study which reported a significant difference in post-test scores of exposed and nonexposed group of students.10 In this study, the mean score in the MCQ based class test of exposed group in all the three cases (hip, knee and combined together of hip and knee) was only slightly higher than that of the non-exposed group. The reason for this may be that all the questions in our MCQ test were not application based and a larger ratio (3:1) of the MCQs were mainly to be answered on recall basis. This may be the reason why both the exposed and nonexposed group of students were able to attempt the questions correctly.
Aside from the above limitations and the additional time and effort needed to conduct this module of ECE with actual patient contact in a supervised setting, the learners were introduced to the most important stakeholder in a healthcare setting i.e. the patient. It not only sensitized and motivated the students,11 but also provided the stimulus and encouragement for self-directed learning. The students learnt about the patient’s perception of illness as well as the impact of the disease on the patients’ families. The students also learnt the technique of interacting with patients thus improving their communication skills besides providing them an insight into the human and social aspects of the practice of medicine. Providing such opportunities for "immersive learning” in the curriculum at an early stage can help commit the learners to patient-centred care, empathy, altruism and service thus helping in smooth transition of the students to the clinical setting.12
ECE in clinical setting has desired impact on the learning of the students, as it gives the student opportunities to be sensitized to the broader context of clinical medicine and encourages them to reflect on their role in addressing the issues of healthcare in the country. With implications like increased interdepartmental collaboration, it has proven to be feasible in our scenario.
Acknowledgement
This study was conducted as part of the FAIMER Fellowship pursued by the corresponding author from CMCL-FRI Ludhiana. We sincerely acknowledge the guidance provided by the FAIMER faculty and colleagues at CMCL-FRI Ludhiana. We also thank the students and the patients without whose participation the project would not have been possible.